As some of you may know, May was Lyme Disease Awareness Month.
Outdooractivities increase in the summertime which makes it a good time to review tick borne disease. Remember where there is nature, there are ticks, and where there are ticks, there exists the possibility of a tickborne disease.
Two families of ticks, Ixodes scapularis (hard bodied ticks) and Argasidae (soft bodied ticks) are responsible for transmitting most tickborne diseases to humans in the US. Once a tick is infected with a pathogen the tick usually survives and is host to the pathogen. Humans are usually incidental hosts, accidentally having the pathogen pass to them during a tick bite, and then carrying the pathogen and contracting an illness.
Ticks effectively transmit the pathogen (bacteria, protozoa, rickettsia, nematodes, and toxins) to humans during the time that the tick is feeding on the human. The feeding site (where the tick bites you and sucks blood) is exposed to infected tick salivary gland secretions and the pathogen is transferred from the tick to the human.
Three species of ticks are responsible for most human disease:
Ixodes scapularis (Blacklegged tick), Amblyomma americanum (Lone Star tick), and Dermacentor variabilis (American dog tick). Each is capable of transmitting multiple pathogens since ticks have no boundaries.
Tick activity is greatest between April and September, but here in California, tick exposure can occur all year round. A CDC report in 2019 showed that tick borne and mosquito-borne infections have tripled over the last 13 years. This includes Lyme disease, which accounts for 82% of all tick-borne diseases.
The CDC now estimates that 476,000 people in the US each year are diagnosed and treated for Lyme disease. Children ages 0-19 years represent 29% of reported Lyme cases from 2001-2017. After a course of treatment, 15-20% or more of patients will have long term symptoms. Many are unaware of the devastating physical, mental, and emotional toll that Lyme disease has.
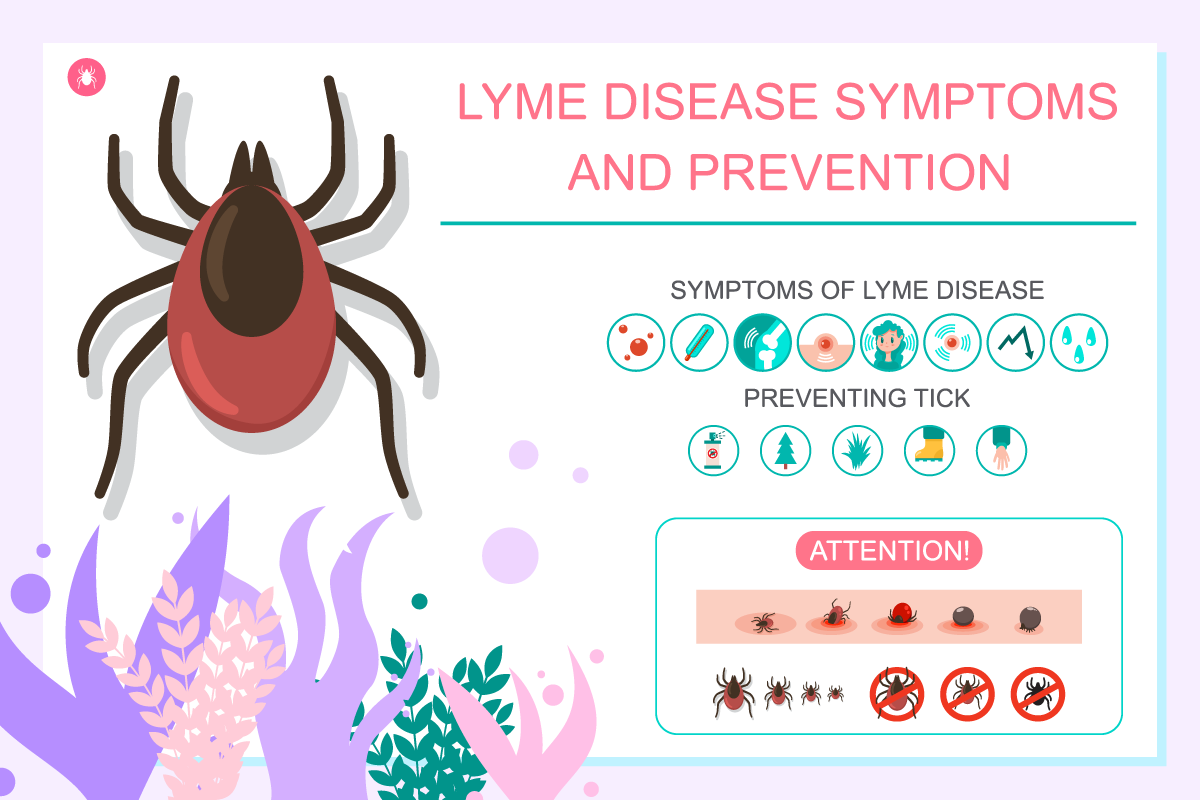
Lyme disease can present as a change in behavior, energy level, appetite, lack of interest in activities you usually love to do, as well as GI symptoms.
Other manifestations including cognitive impairment, mental confusion, memory loss, headaches, difficulty concentrating, speech difficulty, visual and hearing problems, dizziness, mood swings, outbursts, depression, sleep disturbance, OCD, and seizure activity.
With summer fast approaching and people spending more time outdoors, it is important for everyone to learn about and take precautions against ticks and the diseases they carry.
Prevention is the only way to end the tickborne disease epidemic. Education is your best defense against Lyme and other tick-borne diseases.
Outdoors safety tips:
However, if you do contract Lyme disease, if caught early and treated appropriately does NOT have to go on to be a devastating chronic illness. Awareness is key!
The following 6 steps are summarized from Dr. Alexis Chesney’s book, “Preventing Lyme and Other Tick-Borne Diseases.”
Step 1: Immediately Remove and Identify the Tick
Use the O’Tom Tick Twister to remove the tick, identify the tick, and put it in the plastic bag.
Step 2: Apply First Aid
-After you remove the tick, place 2 drops of Andrographis tincture on the tick bite wound.
-Take homeopathic Ledum palustre 30c after a tick bite to encourage healing. (3 pellets under your tongue 3x daily x 3 days)
–Apis mellifica 30c may be added if the tick bite causes a rash or localized swelling which feels hot to the touch, and relieved by cold compresses. Dosage is the same as Ledum palustre.
-After a tick bite, please report the rash to a medical professional.
It is very important to acknowledge that no rash does not mean no disease!
Step 3: Have the Tick Tested for Pathogens
Send the tick to www.tickreport.com or www.ticknology.org for testing.
The turnaround time for both of these labs is around 3 days from receipt of the tick.
Step 4: Begin the Herbal Prophylactic Protocol
For adults, take 1 teaspoon of the Deer Tick Bite Formula (DTBF) in water 3 times a day,
30 minutes before breakfast, lunch, and dinner, for 30 days.
While it is safe to use DTBF with children, the extremely bitter taste is often a deterrent. There are usually more palatable herbal formulas available, some in glycerin base.
Step 5: Watch for Symptoms
Immediately report signs or symptoms of tick-borne diseases to a medical professional.
Step 6: Get Tested (Maybe)
Consult with a medical professional.
Are antibiotics warranted?
Most Lyme-literate practitioners believe that a single dose of doxycycline has never been effective in preventing Lyme disease.
At least a 3-week course of antibiotics is needed to ensure that you kill Borrelia in all of its life forms. By stopping antibiotics too early, you may not kill the Borrelia that is hiding out in its dormant cyst form and waiting for just the right moment to reactivate and convert to its free-floating spirochete form to cause trouble at a future date.
The antibiotic chosen may be herbal, pharmaceutical, or a combination of both.
For adults, a 3-week course of doxycycline may be recommended. There are also alternative antibiotics such as amoxicillin, azithromycin, or cefuroxime if sun sensitivity develops with doxycycline.
Be aware that chronic use of antibiotics can cause fungal overgrowth impacting your gut bacteria..
Herbal anti-microbials targeted to Lyme and co-infections can also be used alone or in combination with pharmaceutical antibiotics. I prefer using herbal anti-microbials due to persister forms & dna transformation of lyme disease that could promote antibiotic resistance. There is also less relapse when using herbs.
Stephen Buhner, a highly regarded Lyme herbalist, recommends the herb Astragalus to boost one’s immune system and prevent Lyme transmission.
After a new tick bite, he recommends the adult dosage of 3000mg daily for 30 days.
For prevention, if you live in a highly endemic Lyme area and don’t want to be on antibiotics for the entire season, Buhner recommends that adults take Astragalus 1000mg daily.
For a 1 year old, you can add 10 drops of the tincture to their diet three times a day. Older children can be given larger doses, around 1/8 tsp, mixed in food daily.
Immediately after a tick bite, Buhner has also found applying a topical paste made of Andrographis tincture and green clay to be helpful in preventing infection.
If you or your child gets bitten by a tick, please discuss what anti-microbial regimen is best with your physician or a Lyme-literate practitioner. (ilads.org)
Wishing you and your family a healthy and happy summer, and do go out and enjoy the great outdoors!
Resources:
Lyme Disease Association (LDA) has a pamphlet written especially for parents and educators called the ABC’s of Lyme Disease.
This pamphlet contains information from experts on the impact of Lyme disease on children’s education, and hundreds of thousands have been distributed.
The LDA also has Tickles, a prevention video, in the “Lyme, Kids and Schools” website section.
National Capital Lyme Disease Association (NatCapLyme) also has an educational and awareness outreach campaign for children and adults called Tick Busters: Wanted Dead or Alive (tickbusters.org). This year their focus is on an awareness and prevention educational program targeting children since they are the most vulnerable population given they play outdoors extensively.